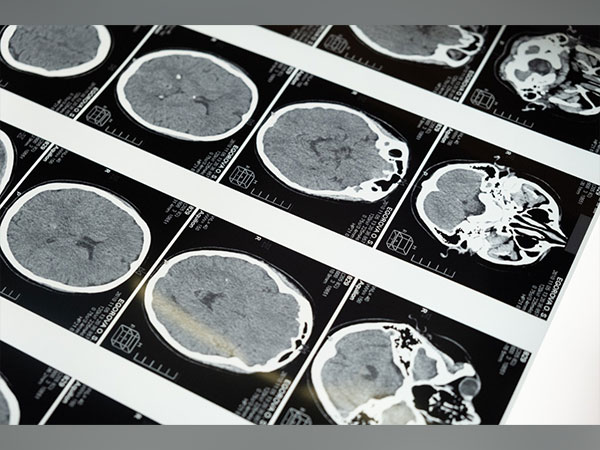
Wisconsin: Like the toughest weed, Glioblastoma almost always returns, typically months after the patient's initial brain tumour is surgically removed. Because of this, the survival rates for this cancer are only 25% after one year and drop to 5% after five years.
The fact that surgeons can't always completely remove all of the tumour or glioma stem cells that may still be present in the brain presents one of the difficulties in treating this illness. "The aggressive nature of the tumour cells in glioblastoma causes them to infiltrate the tissues around them. As a result, it is difficult for the surgeon to distinguish between the tumour and normal tissue, and because all of the brain's tissues are crucial, it is impossible to remove as much as possible," according to Quanyin Hu, an assistant professor in the Pharmaceutical Sciences Division of the University of Wisconsin-Madison School of Pharmacy. Because of this, the likelihood that the tumour will return after treatment is complete dramatically decreases.
But Hu's Cell-Inspired Personalized Therapeutic (CIPT) Lab has created a potent postoperative immunity booster that may change the chances for glioblastoma patients. This month, Hu and his colleagues published their findings in the journal Science Translational Medicine regarding the application of the therapy in mouse models of human glioblastoma.
According to Hu, "it offers hope for avoiding glioblastoma relapse." "We demonstrate that it is capable of eliminating these glioma stem cells, ultimately preventing the recurrence of the glioblastoma. We can greatly increase survival.
A hydrogel that can be injected into the brain cavity left behind by the removed tumour was created by Hu's lab. According to Hu, the hydrogel delivery method is effective because it completely fills the brain cavity, gradually releases the medication into the surrounding tissue, and stimulates the immune system's ability to fight cancer.
The hydrogel is loaded with nanoparticles made to enter and rewire specific immune cell types known as macrophages. In the tumour environment, these immune cells can transform into a form that instead suppresses the immune system and aids in the development of cancer. Normally, these immune cells clear the body of infectious invaders. These rogue macrophages also congregate at the surgical site as a result of the inflammation caused by surgery, which may encourage cancer relapse.
"We want to take advantage of these macrophages and turn them from enemy to ally," Hu said.
To achieve this, the nanoparticles can programme the macrophages to target the cancer stem cell marker CD133, a glycoprotein. Additionally, Hu's team included an antibody called CD47 that disables a "don't eat me" signal to help macrophages detect the cancer cells. The hydrogel treatment successfully produced glioma stem cell-specific chimeric antigen receptor (CAR) macrophages, according to preclinical results in mouse models. This effectively modified the local immune system to find and eliminate any remaining glioma stem cells.
If successful in people, the hydrogel treatment could do away with the need for postoperative radiation or chemotherapy, minimising harmful side effects while also improving patient outcomes.
The hydrogel will be tested in larger animal models in Hu's upcoming research, and he will also keep an eye on its long-term efficacy and toxicity beyond the four to six months he previously examined.
Hu says, "We feel confident that this is a very promising approach for bringing new hope to patients with glioblastoma so they can recover after surgery." However, there is still much work to be done before it could possibly be translated into the clinic. "We hope we can complete our tasks so that this technology can be advanced to the clinic."
Although Hu's team is initially concentrating on glioblastoma, he points out that the therapeutic strategy could also be used to treat other aggressive solid tumours, such as breast cancer. "Our strategy is to locally engineer these macrophages and to take advantage of the macrophages in the postsurgical areas," he claims. "We are confident that the majority of solid tumours with high invasive characteristics will fall under this scenario."